Understanding Pancreatitis Causes, Symptoms, and Treatment
Learn about pancreatitis, its symptoms, diagnosis, causes, and treatment options for effective digestive health recovery.

Pancreatitis
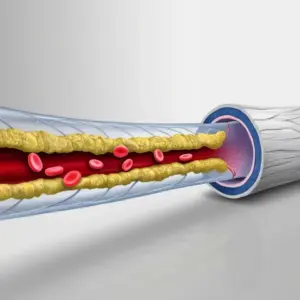
Pancreatitis is an inflammatory condition of the pancreas — an essential gland located behind the stomach that helps in digestion and blood sugar regulation. The pancreas produces digestive enzymes and hormones like insulin and glucagon. When these enzymes become active inside the pancreas instead of the small intestine, they begin to digest the gland itself, causing inflammation and pain.
Pancreatitis can occur suddenly (acute pancreatitis) or develop over time (chronic pancreatitis). If not treated promptly, it can lead to complications such as infection, diabetes, or even pancreatic cancer.
At VS Hospitals, a team of expert gastroenterologists, surgeons, and nutritionists provide advanced care for pancreatitis. Using modern diagnostic tools and evidence-based treatments, the hospital focuses on relieving symptoms, healing the pancreas, and preventing recurrence.

Early Detection Saves Lives
Early detection and treatment are crucial for improving the chances of survival. If you notice any concerning symptoms, consult a healthcare provider immediately.
Signs and Symptoms
Severe abdominal pain
Usually in the upper abdomen and radiating to the back; worsens after meals.
Nausea and vomiting
Caused by digestive disruption and inflammation.
Abdominal tenderness or swelling
Due to fluid buildup around the pancreas.
Fever and elevated heart rate
Indicate infection or severe inflammation.
Loss of appetite
Persistent pain and digestive issues reduce food intake.
Fatty or oily stools (steatorrhea)
Result of improper fat digestion.
Weight loss
Caused by malabsorption and poor appetite.
Jaundice
Yellowing of skin or eyes, especially in bile duct obstruction.
Weakness and fatigue
Due to nutrient loss and dehydration.
Blood in Urine
Hematuria - pink, red, or dark urine, the most common symptom
Frequent Urination
Feeling the need to urinate frequently, even when bladder is not full
Painful Urination
Experiencing pain or burning sensation while urinating
Back or Pelvic Pain
Pain that occurs as the cancer grows and spreads
Unexplained Weight Loss
Significant weight loss not related to diet or exercise
Fatigue
Feeling unusually tired or weak without a clear cause
Meet Our Expert Pancreatitis Treatment specialists
Risk Factors
Smoking
Smoking is one of the leading causes of bladder cancer. Chemicals in tobacco smoke can damage the lining of the bladder, increasing the risk.

Gender
Men are at a higher risk of developing bladder cancer than women.

Chronic Bladder Infections or Inflammation
Conditions such as bladder infections and long-term bladder inflammation can increase the risk.

Exposure to Chemicals
Prolonged exposure to certain chemicals, especially those used in the dye industry, rubber production, and chemical manufacturing, increases the risk.

Gallstones
The most common cause of acute pancreatitis; they block the pancreatic duct.

Excessive alcohol consumption
Damages pancreatic tissue over time, leading to chronic pancreatitis.

High triglyceride levels
Can trigger acute inflammation.
Certain medications
Such as steroids, diuretics, or antibiotics that may irritate the pancreas.

Smoking
Increases the risk of both acute and chronic pancreatitis.

Family history
Genetic predisposition to pancreatic enzyme abnormalities.

Infections or autoimmune conditions
Cause inflammation of pancreatic tissues.

Abdominal trauma or surgery
May injure the pancreas or its ducts.

Uncontrolled diabetes
Prolonged high blood sugar can strain the pancreas.

Obesity
Leads to fat buildup and increased pressure on digestive organs.

Pancreatitis
Diet and Nutrition
Prevention
Diagnosis
Key Services
Key Facilities
Nutrition plays a crucial role in both the management and recovery of pancreatitis. The Diet and Nutrition Department at VS Hospitals works closely with gastroenterologists to design patient-specific dietary plans:
- Low-Fat Diet: Reduces the workload on the pancreas and prevents enzyme overactivation.
- Small, Frequent Meals: Helps improve digestion and minimizes stress on the pancreas.
- High-Protein, Nutrient-Rich Foods: Include lean meats, tofu, and legumes to rebuild tissue.
- Hydration: Drinking plenty of water supports recovery and prevents dehydration.
- Avoid Alcohol Completely: Alcohol can trigger or worsen inflammation.
- Limit Fried and Greasy Foods: These increase fat content and trigger enzyme flare-ups.
- Include Antioxidant Foods: Berries, spinach, and nuts reduce oxidative stress.
- Opt for Steamed or Boiled Meals: Easier to digest than fried or spicy foods.
- Avoid Caffeine and Sugary Drinks: Both can dehydrate and irritate the digestive system.
- Vitamin Supplementation: Vitamins A, D, E, and K may be prescribed for malabsorption cases.
At VS Hospitals, nutrition therapy is tailored to each patient’s medical condition — ensuring balanced healing and long-term pancreatic protection.
While not all causes of pancreatitis can be avoided, adopting preventive measures reduces risk and prevents recurrence. The Gastroenterology team at VS Hospitals recommends the following prevention steps:
- Limit Alcohol Consumption: Avoid alcohol completely to protect pancreatic cells.
- Maintain Healthy Weight: Prevent gallstones and fatty liver by exercising regularly.
- Quit Smoking: Smoking doubles the risk of chronic pancreatitis.
- Eat a Balanced Diet: Low in fat and high in fiber to support digestion.
- Control Triglycerides: Regular monitoring and diet modification to prevent lipid buildup.
- Stay Hydrated: Water helps flush out toxins and supports enzyme activity.
- Avoid Self-Medication: Certain drugs can irritate the pancreas; consult your doctor first.
- Monitor Liver Health: Regular scans and tests for those with gallstones or liver issues.
- Regular Health Check-Ups: Especially for those with family history or past pancreatitis.
- Stress Management: Yoga and relaxation techniques help reduce digestive tension.
At VS Hospitals, prevention programs focus on patient education, lifestyle counseling, and routine screenings to reduce recurrence and promote digestive wellness.
Diagnosing pancreatitis involves detailed clinical examination and advanced imaging tests to determine the severity and cause. VS Hospitals offers comprehensive diagnostic facilities to ensure accurate and rapid diagnosis.
- Physical Examination: Evaluation of upper abdominal tenderness, swelling, and pain, along with reviewing medical history, alcohol intake, and previous digestive or gallbladder issues.
- Blood Tests: Measurement of amylase and lipase enzyme levels to confirm inflammation, along with liver function, calcium, and blood sugar tests for complication assessment.
- Imaging Tests: Ultrasound to detect gallstones or duct blockages; CT scan and MRI/MRCP for identifying inflammation, necrosis, and detailed pancreatic duct visualization.
- Endoscopic Ultrasound (EUS): Provides high-resolution images of the pancreas and surrounding structures, allowing early detection of minor abnormalities or hidden lesions.
- Stool Tests: Used to assess fat malabsorption, digestive enzyme deficiency, and chronic pancreatic dysfunction, supporting diagnosis of long-term pancreatitis cases.
- Biopsy (If Required): Performed to analyze pancreatic tissue, helping rule out malignancy or chronic fibrotic changes for precise disease characterization.
At VS Hospitals, the diagnostic process is handled by experienced gastroenterologists and radiologists using advanced imaging systems to ensure timely and precise detection.
VS Hospitals provides specialized and comprehensive care for patients with pancreatitis focusing on both immediate treatment and long-term prevention.
- Acute Pancreatitis Management: Hospitalization with IV fluids for hydration, advanced pain management, and gradual oral feeding under dietitian guidance; ERCP performed for gallstone-related duct blockages.
- Chronic Pancreatitis Care: Includes pancreatic enzyme replacement for digestion, insulin therapy for diabetes, surgical tissue removal if needed, and lifestyle counseling to prevent recurrence.
- Minimally Invasive Procedures: ERCP and EUS-guided drainage effectively treat duct obstructions and pseudocysts, while laparoscopic surgery ensures reduced pain, minimal scarring, and faster recovery.
- Nutritional and Rehabilitation Support: Personalized low-fat, high-protein diets with essential vitamin and mineral supplementation to restore nutrition and maintain optimal digestive function.
- Emergency and Intensive Care: 24/7 ICU support for severe pancreatitis, continuous fluid and oxygen monitoring, and advanced life-support systems for critical multi-organ conditions.
- Comprehensive Long-Term Management: Regular follow-ups, preventive screenings, and patient education to reduce recurrence risk and ensure sustained pancreatic health.
At VS Hospitals, the treatment approach combines cutting-edge technology with compassionate care to ensure patients recover faster and reduce recurrence risk.
VS Hospitals offers a world-class gastroenterology setup designed for accurate diagnosis, safe treatment, and comfortable recovery for patients with pancreatitis.
- Advanced Gastroenterology Department: Equipped with the latest endoscopic and imaging tools.
- High-Resolution Imaging Suite: Includes MRI, CT scan, and ultrasound systems for detailed evaluation.
- Endoscopy and ERCP Unit: For both diagnostic and therapeutic procedures.
- 24/7 Intensive Care Unit (ICU): For managing acute and critical pancreatitis cases.
- Comprehensive Laboratory Services: On-site testing for enzymes, liver profile, and infection markers.
- Robotic and Laparoscopic Surgery Unit: Minimally invasive options for surgical management.
- Dedicated Nutrition and Diet Counseling Center: Tailored meal plans for pancreatic recovery.
- Emergency Response Team: Round-the-clock care for life-threatening pancreatitis complications.
- Post-Treatment Rehabilitation Program: Focused on recovery, lifestyle modification, and follow-up.
- Multidisciplinary Care Collaboration: Gastroenterologists, surgeons, endocrinologists, and dietitians work together for holistic treatment.
With these facilities, VS Hospitals stands as one of the leading centers for pancreatic and gastrointestinal care in Chennai, ensuring precision, comfort, and complete recovery for every patient.
Top Medical Facilities at Our Multispeciality Hospital – Here’s What Makes Us Different!
Ready to Begin Your Pancreatitis Care Journey?
Learn More About Pancreatitis Care
Frequently Asked Questions
Pancreatitis is caused mainly by gallstones, alcohol abuse, or high triglyceride levels. It ranges from mild inflammation to life-threatening conditions. At VS Hospitals, doctors use advanced imaging and lab tests to diagnose the cause early and initiate effective treatment to prevent organ damage or chronic complications.
Treatment at VS Hospitals focuses on pain relief, enzyme management, and restoring digestion. Acute cases receive IV fluids, nutrition therapy, and endoscopic procedures for duct clearance. Chronic cases may require enzyme replacement or surgery. The team ensures comprehensive care and lifestyle counseling for long-term recovery.
Yes, prevention is possible through lifestyle changes. Avoid alcohol, maintain healthy triglyceride levels, and eat a balanced diet. VS Hospitals provides personalized wellness programs, diet counseling, and regular screenings that help identify risks early and prevent recurrence of pancreatitis and related complications.
