Hypertensive nephropathy treatment plays a crucial role in managing kidney damage caused by prolonged high blood pressure. This condition, if left untreated, can lead to progressive kidney failure, significantly impacting quality of life. At VS Hospitals, our approach to hypertensive nephropathy treatment combines advanced medical interventions with personalized care, aiming to control blood pressure, reduce symptoms, and protect kidney function. Understanding and treating this condition early is key to better health outcomes.
Understanding Hypertensive Nephrosclerosis
Hypertensive nephrosclerosis, often referred to as hypertensive nephropathy, is a condition where persistent high blood pressure damages the small blood vessels in the kidneys, reducing their ability to filter waste from the blood. This progressive damage often leads to hypertensive nephropathy stages that, if left untreated, can culminate in end-stage renal disease. Key aspects include:
- Blood vessel damage: High blood pressure injures tiny kidney blood vessels, impairing function.
- Loss of kidney filtration: Reduced efficiency in removing waste and excess fluids.
Early hypertensive nephropathy treatment, focused on lowering blood pressure and protecting kidney function, can slow or even prevent further damage, greatly benefiting long-term kidney health.
Hypertensive Nephropathy Treatment
At VS Hospitals, hypertensive nephropathy treatment focuses on comprehensive management to slow disease progression and preserve kidney function. This approach combines medications, lifestyle changes, and consistent monitoring, creating an effective plan for long-term health.
- Blood Pressure Control: Medications like ACE inhibitors and ARBs are commonly used to keep blood pressure in check, reducing the strain on kidneys and slowing damage.
- Proteinuria Management: Elevated protein in the urine can accelerate kidney damage. Treatment may include specific medications and dietary adjustments to lower protein levels, helping protect the kidneys.
- Glycemic Control: For patients with diabetes, controlling blood sugar is vital to prevent complications. Balanced diets, medications, and regular monitoring ensure optimal blood sugar levels.
- Routine Monitoring: Regular kidney function tests and blood pressure checks allow early detection of changes, enabling timely adjustments to the treatment plan.
This integrated approach to hypertension kidney transplant not only manages current symptoms but also helps improve overall health, providing patients with a higher quality of life.
Causes of Hypertensive Nephropathy
Hypertensive nephropathy is primarily caused by long-term high blood pressure that damages the small blood vessels in the kidneys. This damage gradually impairs the kidneys’ ability to filter waste from the blood, leading to best hypertension medication for kidney disease. Several factors contribute to developing hypertensive nephropathy:
- Chronic Hypertension: Prolonged high blood pressure stresses the kidneys, making them vulnerable to damage.
- Genetic Predisposition: Family history of hypertension after kidney transplant or kidney disease can increase the risk.
- Diabetes: High blood sugar levels, when combined with hypertension kidney transplant, accelerate kidney damage.
Addressing these causes through effective hypertensive nephropathy treatment can prevent further kidney complications.
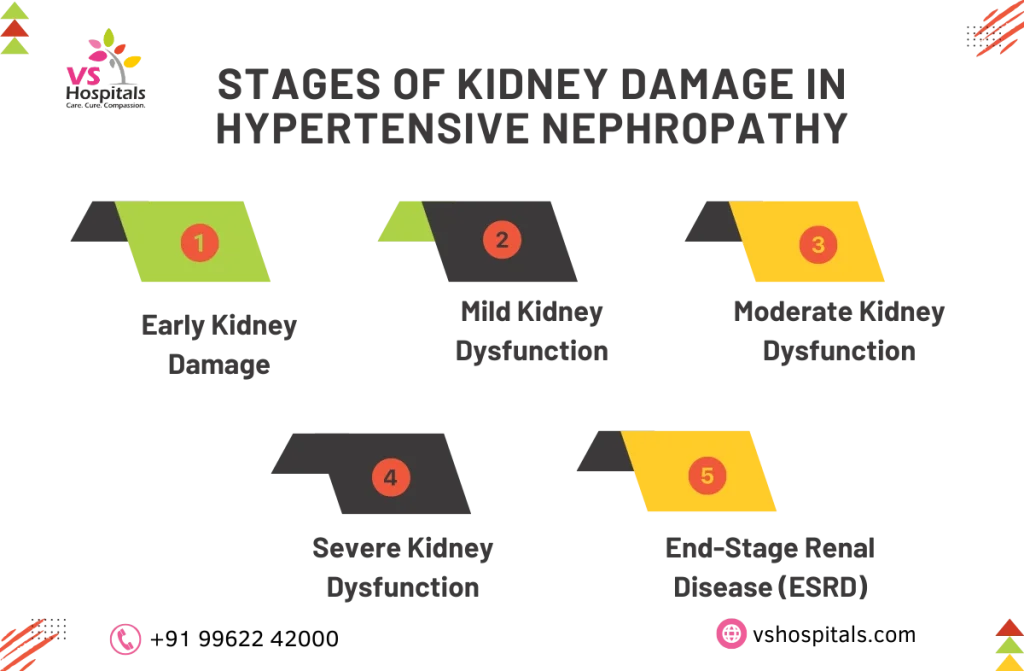
Hypertensive Nephropathy Stages
Hypertensive nephropathy treatment is tailored according to the stage of kidney function decline. Each stage reflects the level of kidney damage and requires specific care strategies to manage symptoms and prevent progression. Here’s a breakdown of the stages:
- Stage 1: Kidneys function normally or have only slight reductions in filtration. Lifestyle changes and regular monitoring are vital.
- Stage 2: Moderate reduction in Glomerular Filtration Rate (GFR); medications are often introduced to control blood pressure and reduce proteinuria.
- Stage 3: Noticeable decline in GFR; symptoms intensify, requiring intensified hypertensive nephropathy treatment.
- Stage 4: Severe GFR reduction; preparations for dialysis or transplant may begin.
- Stage 5 (End-Stage Renal Disease): Requires dialysis or hypertension after kidney transplant for survival.
Conclusion
Hypertensive nephropathy treatment is essential to prevent kidney function from worsening and to maintain a good quality of life. By focusing on blood pressure management, proteinuria reduction, and regular monitoring, VS Hospitals offers comprehensive care to address each stage of the best hypertension medication for kidney disease. Taking action early is critical to slow disease progression, and our specialized team is dedicated to supporting patients every step of the way for better outcomes and a healthier future.
Read also Best exercises for kidney health
