Genetic testing for Cancer is a groundbreaking method that helps identify inherited mutations which may increase an individual’s risk for certain types of cancer. At VS Hospitals, we recognize the importance of this test in providing patients with tailored care. This innovative process allows individuals to understand their genetic makeup, offering insight into potential health risks, and helping healthcare providers recommend preventive measures, personalized screenings, and treatments. In this article, we will explore what genetic testing is, the benefits, how it works, and who should consider it.
What is Genetic Testing for Cancer?
Genetic testing for cancer involves analyzing a person’s DNA to identify genetic mutations that may make them more likely to develop certain types of cancer. These mutations are often inherited from a parent, and the test can help determine whether a person carries a genetic predisposition to specific cancers, such as breast, ovarian, or colorectal cancer.
- Gene Mutations: Genetic testing typically looks for changes in specific genes that are linked to cancer, such as BRCA1, BRCA2, and others. If these genes are mutated, the risk of developing cancers such as breast, ovarian, or prostate cancer may increase.
- Early Detection: By identifying these mutations early, individuals can make informed decisions about screenings, preventative measures, and lifestyle changes that can reduce their risk of developing cancer.
- Personalized Approach: Genetic testing allows doctors to create personalized prevention or treatment plans based on an individual’s genetic risk factors.
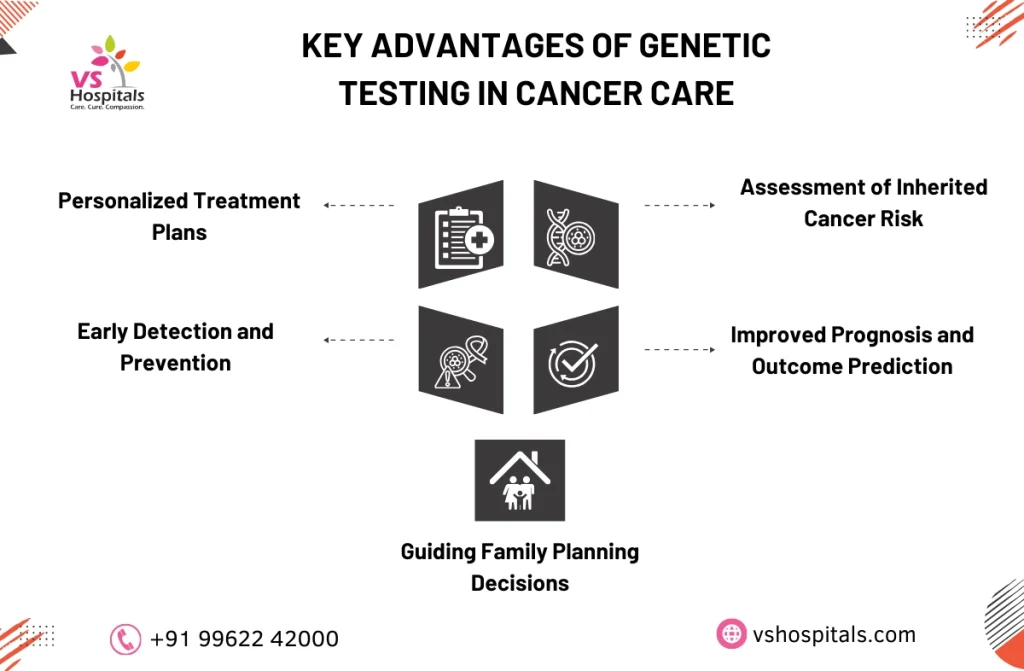
Benefits of Genetic Testing for Cancer
The benefits of genetic testing extend far beyond simply identifying a risk. This tool can help in early diagnosis, prevention, and the development of personalized treatment strategies.
- Proactive Health Measures: Knowing about genetic predispositions allows individuals to take early action, such as more frequent screenings or preventive surgeries, to reduce cancer risks.
- Personalized Treatment: When genetic mutations are identified, treatments can be tailored to a patient’s genetic profile, improving their effectiveness. This approach is particularly valuable for patients diagnosed with cancer, as genetic testing for cancer treatment can help doctors determine the most effective course of action.
- Family Health: Genetic testing for cancer can reveal whether family members are at increased risk. If a mutation is found, relatives can also be tested to determine their genetic risks.
If you’re considering comprehensive support in your cancer journey, you might want to consult the best surgical oncologist, known for precise treatment plans and high success rates. Understanding the benefits of genetic testing for cancer can also guide personalized care and proactive risk management.
Genetic Testing for Cancer Risk
Genetic testing is crucial for identifying inherited mutations that can increase the likelihood of developing cancer. It is especially important for individuals who have a family history of cancer or those who have been diagnosed with a type of cancer that could be linked to genetic mutations.
- Family History: If multiple family members have been diagnosed with the same type of cancer, genetic testing for cancer can help understand whether the risk is hereditary.
- Understanding Risk Levels: By testing for specific gene mutations, individuals can better understand their risk level and take preventive steps, such as increased screenings or medications.
- Early Interventions: With the right knowledge, individuals can undergo regular screenings at an earlier age, potentially detecting cancer at a stage when it is easier to treat.
Who Should Consider Genetic Testing for Cancer?
Genetic testing is not for everyone, but it is especially valuable for certain groups. People with a family history of cancer, or those diagnosed with cancer at a young age, should consider undergoing genetic testing.
- Family History of Cancer: If there is a history of cancer, particularly cancers that are linked to genetic mutations (like breast or colon cancer), testing can provide valuable insight into personal risks.
- Young Cancer Diagnoses: Individuals who are diagnosed with cancer at a young age may benefit from genetic testing to understand if a genetic mutation is responsible for their condition.
- Known Inherited Mutations: Those who know they carry certain inherited mutations, such as BRCA1 or BRCA2, should consider genetic testing to assess the risk for developing other types of cancer.
For patients also managing related conditions, such as kidney disorders, it’s essential to understand the best foods for kidney disease, as diet plays a critical role in long-term health management.
Understanding the Genetic Testing for Cancer Cost
The cost of genetic testing for cancer can vary depending on the type of test and the laboratory used. However, many patients find that the potential benefits of understanding their genetic risks far outweigh the costs.
- Insurance Coverage: In many cases, health insurance may cover genetic testing, especially if it is recommended by a doctor based on family history or personal health conditions.
- Cost Factors: The price for genetic testing can range from a few hundred to several thousand dollars, depending on the test’s complexity.
- Long-Term Savings: While the upfront cost of genetic testing may seem high, the long-term savings from preventive measures, early cancer detection, and personalized treatments can be significant.
At VS Hospitals, we assist patients in navigating the costs of genetic testing for cancer, ensuring that the genetic testing for cancer cost is both accessible and valuable in the long run. In addition to genetic insights, lifestyle factors like bone health play a major role in survivorship. Learn about bone health in women to support overall well-being.
What to Expect During Genetic Testing
The process of genetic testing is straightforward, and most tests involve collecting a sample of blood or saliva. Here’s what you can expect during the test:
- Consultation: Before the test, you’ll meet with a genetic counselor or healthcare provider who will review your family history and help determine which tests are appropriate.
- Sample Collection: The test typically involves a blood draw or a saliva sample. The sample is sent to a laboratory for analysis.
- Result Interpretation: Once the test results come back, your doctor or genetic counselor will go over them with you and help interpret what the findings mean for your health. These results can also guide genetic testing for cancer treatment to help determine a more personalized care plan.
What Do the Results of Genetic Testing Mean?
The results of genetic testing can be life-changing, offering insights into an individual’s genetic predisposition to cancer.
- Positive Result: If a genetic mutation is found, it may indicate an increased risk for certain cancers. However, this doesn’t mean they will definitely develop cancer. Preventive steps and early detection can still help mitigate risks.
- Negative Result: If no mutations are found, it suggests that you may not have a heightened genetic risk for certain cancers. However, this does not eliminate the possibility of developing cancer due to other factors, such as lifestyle or environmental exposures.
- Uncertain Result: Sometimes, results may show mutations that are not well understood. These are called variants of uncertain significance (VUS), and further monitoring may be recommended.
Conclusion
Genetic testing for cancer is an essential tool in modern healthcare, offering valuable insights into cancer risks, prevention, and treatment. At VS Hospitals, we understand how crucial it is for patients to have access to personalized information about their genetic makeup. This knowledge can lead to better prevention strategies, earlier diagnoses, and more effective treatments. Whether you’re considering genetic testing to assess your risk or to explore potential treatment options, we encourage you to take the next step in understanding your health better. It is a powerful ally in the fight against cancer, offering hope and empowerment for the future.
Read also Cancer death rate in India
