Simply put, dialysis is a treatment that takes over the job of the kidneys by removing toxins, excess waste, and fluids from the body. But there’s more than one way to perform this life-saving procedure.The 2 types of dialysis—hemodialysis and peritoneal dialysis—offer distinct approaches to managing kidney failure. At VS Hospital, we provide both options, ensuring you receive the care that suits your lifestyle and health needs.
What Is Dialysis?
Dialysis replaces the natural filtering process of the kidneys when they can no longer function effectively. The 2 types of dialysis ensure your blood remains clean, your body stays balanced, and complications are minimized. At VS Hospital, our specialists not only perform these procedures but also educate patients on the processes, benefits, and risks, empowering you to actively participate in your care journey.
What Are the 2 Types of Dialysis?
The 2 types of dialysis—hemodialysis and peritoneal dialysis—offer distinct approaches to managing kidney failure. Your medical team will guide you toward the best option for your condition and lifestyle.
Hemodialysis
This method involves cleaning your blood outside the body using a dialysis machine. It is highly effective for individuals with severe kidney failure and typically requires regular visits to a hospital or dialysis center.
Peritoneal Dialysis
This home-based treatment uses a special fluid introduced into your abdomen to remove waste and excess fluids. It offers greater flexibility and independence for those who prefer to manage their treatment at home.
Both types of dialysis are available at VS Hospital, where trained specialists prioritize safety, comfort, and efficiency.
Hemodialysis: The First Type of Dialysis
Hemodialysis, one of the 2 types of dialysis, involves the use of a dialysis machine and an artificial kidney (dialyzer) to clean your blood.
- How It Works: Blood is drawn through a needle inserted into a blood vessel, filtered through the machine to remove toxins, and then returned to your body.
- Frequency: Typically performed three times a week, with each session lasting about four hours.
- Benefits: It efficiently removes toxins and excess fluids, making it ideal for severe kidney failure patients.
At VS Hospital, state-of-the-art facilities and a caring environment ensure every hemodialysis session is as stress-free as possible.
Peritoneal Dialysis: The Second Type of Dialysis
The second option among the 2 types of dialysis is peritoneal dialysis, a treatment designed for flexibility and independence.
- How It Works: A catheter is placed in your abdomen, and a special fluid is used to absorb waste and excess fluids through the peritoneal membrane.
- Frequency: Can be performed multiple times daily (manual exchanges) or overnight using an automated machine.
- Advantages: This method allows patients to undergo treatment at home, avoiding the need for frequent hospital visits.
VS Hospital provides comprehensive training to help patients perform peritoneal dialysis safely and confidently at home.
What Happens After Dialysis?
After Hemodialysis Care
Proper after dialysis care is vital for maintaining health and preventing complications.
- Rest and Hydration:
- Adequate Rest: Post-dialysis fatigue is common. Short naps or relaxation can help replenish energy levels.
- Hydration: Drinking water within recommended limits helps combat dehydration and stabilize blood pressure.
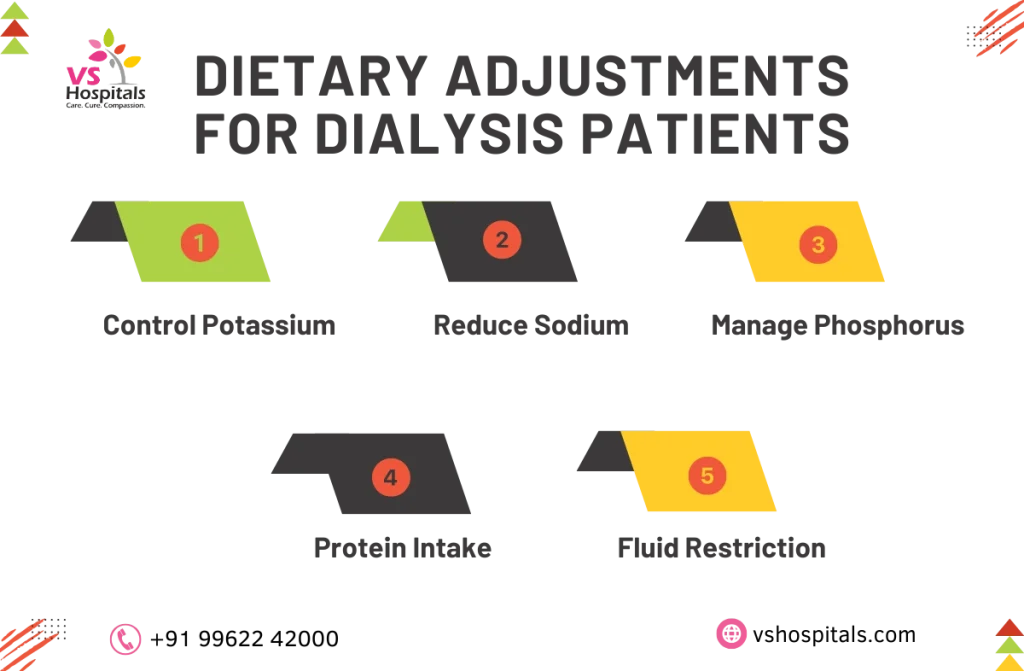
- Dietary Adjustments:
- Low Potassium and Phosphorus: Focus on foods like apples, rice, and white bread.
- Reduced Sodium: Opt for fresh herbs to enhance flavor without adding salt.
- Protein Balance: Include high-quality protein like eggs, fish, and chicken to maintain muscle strength.
- Monitoring for Symptoms:
- Infection Signs: Look for redness, swelling, or discharge at needle sites.
- Discomfort: Report persistent pain or unusual symptoms to your healthcare provider.
learn more about HMPV treatment in Chennai if you experience symptoms like coughing or breathing difficulties.
After Peritoneal Dialysis Care
For peritoneal dialysis patients, after dialysis care is equally essential to maintain safety and effectiveness.
- Catheter Site Care:
- Daily Hygiene: Clean the site with mild soap or antiseptic solutions.
- Regular Monitoring: Watch for redness, swelling, or other signs of infection.
- Diet and Fluid Management:
- Reduce Sodium: Lower salt intake to avoid fluid retention.
- Manage Fluids: Stick to recommended limits to prevent strain on the body.
- Post-Dialysis Syndrome Management:
- Adjust Fluid Concentration: Collaborate with your care team to ensure the correct balance.
- Gradual Dialysis: Slower sessions reduce rapid fluid shifts.
- Hydration (Within Limits): Proper hydration can ease discomfort.
At VS Hospital, we provide emotional support, nutritional guidance, and regular health monitoring to ensure comprehensive after dialysis care. If you’re also managing liver health, consider exploring natural remedies for fatty liver to support overall well-being.
Hospice Care Dialysis: A Personalized Approach
For patients in hospice care, dialysis can be tailored to focus on comfort and quality of life.
- Customized Treatment: Hospice care dialysis prioritizes symptom management and aligns with the patient’s needs and preferences.
- Holistic Support: Our team addresses physical and emotional well-being, ensuring dignity and care at every stage.
At VS Hospital, hospice care dialysis emphasizes patient-centered solutions to improve overall well-being.
Risks and Benefits of the 2 Types of Dialysis
Understanding the risks and benefits of dialysis helps you make informed decisions:
Hemodialysis
- Benefits: Effective toxin removal, rapid results, and ideal for hospital care.
- Risks: Potential for low blood pressure, infections, or muscle cramps.
Peritoneal Dialysis
- Benefits: Greater flexibility, home-based treatment, and needle-free procedures.
- Risks: Risk of peritonitis (infection) and bloating.
VS Hospital’s advanced facilities and experienced team minimize risks and enhance the benefits of both types of dialysis.
Managing Post-Dialysis Syndrome
Post dialysis syndrome, characterized by symptoms like fatigue, headaches, or cramps, can occur after treatments. At VS Hospital, we offer solutions to manage this condition effectively:
- Hydration and Rest: Resting and consuming fluids within recommended limits help alleviate symptoms.
- Medications: Tailored prescriptions for cramps or blood pressure issues.
- Gradual Dialysis: Adjusting the pace of treatment minimizes sudden fluid or electrolyte shifts.
Regular follow-ups ensure patients are monitored for post dialysis syndrome, preventing complications and enhancing recovery.
Are There Any Activity Limitations During Dialysis?
Undergoing dialysis does not mean you have to give up your daily activities completely. However, certain activity restrictions are necessary to avoid complications like post dialysis syndrome. Here’s how you can stay active safely:
- Light Exercise: Engage in low-impact activities like walking, yoga, or stretching to maintain mobility.
- Avoid Heavy Lifting: Refrain from lifting heavy objects, as it can strain your muscles and affect your dialysis access site.
- Stay Hydrated: Follow fluid intake recommendations to prevent dehydration, which can worsen post dialysis syndrome.
- Listen to Your Body: If you experience fatigue, dizziness, or weakness, rest and avoid strenuous activities.
- Consult Your Doctor: Discuss safe activity levels with your healthcare provider to prevent complications.
By balancing activity with rest, you can maintain your physical well-being while managing dialysis effectively.
Conclusion
Understanding the 2 types of dialysis—hemodialysis and peritoneal dialysis—allows you to make informed decisions for managing kidney health. At VS Hospital, our dedicated team ensures a seamless experience, addressing every aspect of your care journey. For patients experiencing post dialysis syndrome, we provide tailored care plans to alleviate symptoms and improve quality of life. Whether it’s routine dialysis or hospice care dialysis, our expert team is here to guide you every step of the way.
Read also Risk Factors for Cancer
