Chronic kidney disease treatments are essential for managing the progression of kidney issues, improving life quality, and addressing symptoms effectively. These treatments focus on slowing disease progression, reducing complications, and helping patients lead healthier lives. By understanding available treatment options and taking proactive measures, individuals with chronic kidney disease can navigate their journey with greater resilience and support. At VS Hospitals, we’re committed to providing comprehensive, patient-centered treatment options tailored to each stage of kidney disease.
Symptoms of Chronic Kidney Disease
Recognizing the symptoms of chronic kidney disease early on is key to effective management and timely intervention. As kidney function declines, a range of symptoms may gradually appear, often becoming more noticeable in later stages. Common symptoms include:
- Fatigue and weakness: Reduced kidney function affects energy levels.
- Swelling: Fluid retention may cause swelling in the ankles, feet, or face.
- Nausea and vomiting: Waste buildup can lead to gastrointestinal issues.
- Frequent urination: Often more noticeable at night.
- Muscle cramps: Imbalance in minerals leads to cramps and discomfort.
Identifying these symptoms promptly is essential for seeking chronic kidney disease treatments and slowing disease progression.
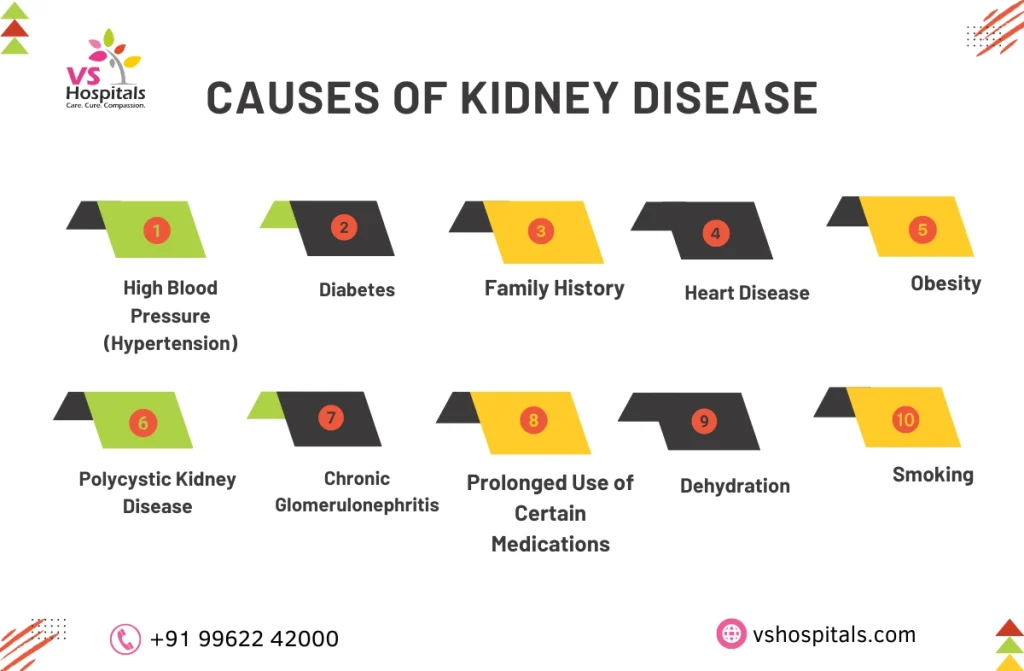
Causes of Kidney Disease
Understanding the root causes of kidney disease is crucial in managing and preventing the condition effectively. Chronic kidney disease often arises from a combination of lifestyle, medical, and genetic factors that impact kidney function over time. Common causes include:
- High Blood Pressure: Persistent high blood pressure damages the small blood vessels in the kidneys.
- Diabetes: Elevated blood sugar levels harm the kidneys’ filtering units.
- Family History: A genetic predisposition to kidney disease can increase risk.
- Heart Disease: A weakened heart reduces blood flow, impacting kidney function.
Each of these factors contributes to the onset of kidney disease, highlighting the importance of chronic kidney disease self care and preventive treatments.
Stages of Kidney Failure
Chronic kidney disease treatments vary according to the stages of kidney failure, with each stage reflecting a different level of kidney function. The disease progresses through five main stages, each with distinct symptoms and treatment needs.
- Stage 1: Kidneys are damaged but function normally (90% or more); few or no symptoms.
- Stage 2: Mild decrease in kidney function (60-89%); some signs of kidney stress.
- Stage 3: Moderate decrease in function (30-59%); common symptoms include swelling and fatigue.
- Stage 4: Severe reduction (15-29%); requires more intensive treatment.
- Stage 5: Advanced kidney failure (below 15%); dialysis or transplant is needed.
Recognizing these stages of kidney failure helps guide appropriate chronic kidney disease treatments for better outcomes.
Chronic Kidney Disease Treatments
Chronic kidney disease treatments aim to manage symptoms, slow disease progression, and improve patients’ overall quality of life. At VS Hospitals, our team provides a variety of treatment options based on the stage of kidney disease and individual patient needs. Here’s an overview of common treatment methods:
- Medications: Control blood pressure and prevent further kidney damage.
- Dietary Changes: Low-sodium and low-protein diets to reduce kidney strain.
- Dialysis: Filters waste from the blood for advanced stages.
- Lifestyle Adjustments: Regular exercise, avoiding smoking, and limiting alcohol.
- Kidney Transplant: A potential solution for end-stage kidney failure.
These chronic kidney disease treatments help patients maintain health and manage symptoms effectively.
Prevention of Chronic Kidney Disease
Preventing chronic kidney disease (CKD) and practicing effective self-care are vital for maintaining kidney health and slowing disease progression. Key strategies include:
- Healthy Diet: Consume a balanced diet rich in fruits, vegetables, and whole grains, while limiting sodium and processed foods.
- Regular Exercise: Engage in physical activities like walking or cycling to maintain a healthy weight and control blood pressure.
- Routine Check-ups: Schedule regular medical appointments to monitor kidney function, especially if you have risk factors such as diabetes or hypertension.
- Avoid Overuse of Painkillers: Limit the use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, as they can harm the kidneys.
By incorporating these self-care practices, individuals can significantly reduce the risk of developing CKD and manage existing conditions more effectively.
Side Effects of Chronic Kidney Disease
The side effects of chronic kidney disease can impact various areas of the body, making it essential to manage symptoms alongside treatment. As kidney function declines, waste builds up in the blood, leading to multiple complications that affect quality of life and health. Here are some common side effects to be aware of:
- Heart problems: Increased risk of heart disease and high blood pressure.
- Anemia: A reduced red blood cell count due to decreased kidney function.
- Bone health issues: Weak bones and fractures from mineral imbalances.
- Nerve damage: High toxin levels in the blood can cause nerve-related issues.
Addressing these side effects of chronic kidney disease through appropriate treatments and lifestyle adjustments can help improve well-being and prevent further complications.
Conclusion
Chronic kidney disease treatments are vital for maintaining kidney health and enhancing quality of life. By combining medical interventions, lifestyle changes, and preventive care, individuals can effectively manage their condition. At VS Hospitals, we are dedicated to offering comprehensive chronic kidney disease self care, empowering patients and their families to navigate this journey with confidence and support.
